Enrollment Expectations & Timelines Page 6 of 7
Plan Changes & Enrollment Request
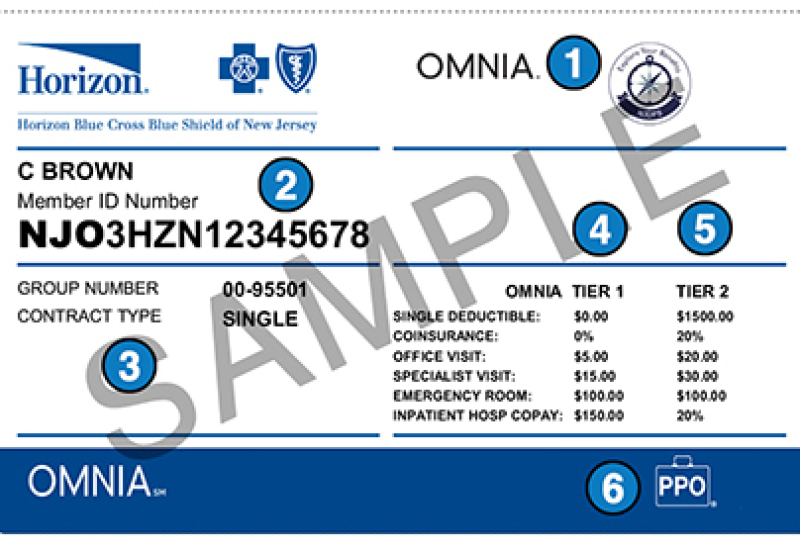
Once your plan change or enrollment request is submitted, carriers take 3-5 days to approve your application. Your Member ID card will arrive by mail in 7-10
business days.
Carriers require 1st month's premium. Credit card or ACH bank payments are accepted. Auto-pay is set up upon enrollment.
1st Month's Premium Payment
Confirm Your Premium Payment. 2-3 days after submitting
your premium payment, check with your bank or credit card activity, once funds are received by the carrier you are approved.
Many times, the 1st Invoice you receive will show you still owe 1st month's premium. Check
with your bank or credit card to confirm premiums were sent to the carrier.
30-day Grace Period: You have a 30-day grace period to pay your Invoice. If termed for late or non-payment, call the Billing Department to submit premiums and request reinstatement.
MEMBER PORTALS
Once you have your Member ID #, you can register and access your online Member Portal.
Carrier Websites - Member Portals:
- HorizonBlue.com
- AmerihealthNJ.com
- HiOscar.com
- Aetna.com
Member Portals to access:
- View plan benefit details
- Update your personal information
- Pay your monthly premium
- View payment history
- Print /re-order ID cards
- View your prescriptions benefits
- View the status of claims
- Health & wellness resources
- Message or Chat features
Member Services:
- Horizon BCBS: 800-355-2583
- Amerihealth: 888-968-7241
- Oscar Insurance: 855-672-2788
- Aetna 800-872-3862
- GetCoveredNJ: 833-677-1010